Diabetic Heel Pain: Causes, Prevention and Treatment Options

If you're experiencing heel pain frequently while also suffering from diabetes, don't be surprised, as heel pain and diabetes often go hand-in-hand. Luckily, you can take many steps to alleviate your pain.
This article will dive deeper into the causes of diabetic heel pain.
What is diabetic heel pain?
Heel pain is one of the symptoms of plantar fasciitis and is a common condition among people with diabetes. There's a high correlation between plantar fasciitis and type 2 diabetes. One of the primary symptoms is pain in the back of the heel, especially when standing up after you wake up in the morning. The pain, unfortunately, may re-occur throughout the day. The pain occurs because of inflammation in the tissue under your foot.
What is plantar fasciitis?
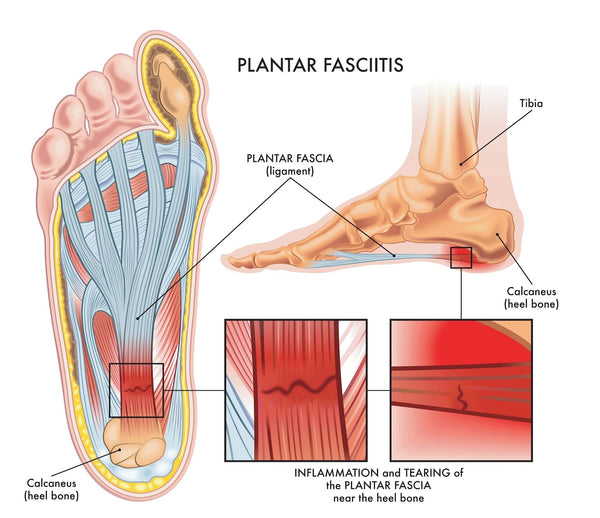
Plantar fasciitis is the most common cause of heel pain, characterized by the inflammation of the plantar fascia. This tough, fibrous tissue stretches across the bottom of the foot, connecting the heel bone to the toes' base and playing a crucial role in maintaining the foot's arch and facilitating smooth walking mechanics.
The plantar fascia experiences increased tension when bearing weight or during the push-off phase while walking or running. These actions are integral to everyday movement but can make the fascia less elastic and more prone to irritation from regular activities over time or with excessive use.
What causes diabetic heel pain?
Plantar fasciitis causes can be attributed to several factors, including:- Age
- Diabetes
- Prior foot conditions
- Obesity
- Standing for extended periods
- Not having the proper equipment/poor form when exercising
Most commonly, people between the ages of 40 and 60 can experience the symptoms of this condition. For people suffering from diabetes, usually, there is an increase in plantar fascia thickness. Some foot conditions, such as flat feet or high arch, can be attributed to heel pain.
In most cases, the primary cause is pressure against the heel. There's too much pressure on the foot, which results in heel pain.
How does peripheral neuropathy cause heel pain?
Peripheral neuropathy impacts the body's nerves, especially in the feet and limbs, leading to symptoms like numbness, a tingling sensation, or even sharp, burning pains. It can also weaken muscles and impair coordination, complicating daily movements and tasks. This condition poses high concern for individuals with diabetes, as elevated blood sugar levels can harm foot nerves and diminish blood circulation in the area. This scenario increases the likelihood of experiencing diabetic heel or foot pain in general, alongside an increased risk for infections and foot-related complications.
Regular inspection for abrasions, ulcers, or injuries is crucial to safeguard your feet from the effects of peripheral neuropathy. Wearing properly fitting, supportive footwear and steering clear of high heels or overly tight shoes is equally important. Those with diabetes should closely collaborate with their medical providers to control blood sugar, mitigating nerve damage and additional complications. Incorporating regular physical activity can aid in maintaining adequate blood circulation to the feet, further minimizing peripheral neuropathy's potential complications. Effective foot care and proactive health management are key to managing the effects of peripheral neuropathy and preventing severe foot issues.
What does diabetic foot pain feel like?
Diabetic foot pain hits the back heel of your foot. People experience it after waking up, standing or sitting for long periods. A stabbing pain goes up to the ankle with some stiffness as well. If you're experiencing any of these symptoms, you should contact a doctor and have your foot checked.
How do you get diabetic heel pain relief?
There are numerous ways to get heel pain relief. Some are immediate treatments, while others are lifestyle changes that will alleviate the symptoms over time.
These treatments & lifestyle changes may include:
1) Body weight: Be mindful of what you place into your body; everything you digest is treated as fuel for your body. You can monitor your blood sugar levels with a well-balanced diet while still losing weight. Lowering your body weight will reduce pressure on your foot. This will result in less pain in the long term.
2) Regular exercise: Exercising will increase your metabolism and is a tool for weight management. Regular exercise will also strengthen muscles and ligaments around your ankles and feet. Having healthier calves will also lower your heel pain. A suggested first step is walking three to four times per week. The ligaments and muscles will strengthen over time as your frequency increases.
3) Visit a foot doctor: Visit a foot doctor. A specialist might suggest specific shoes or different orthoses as a solution. For example, wearing a night splint might lower the pain.
4) Make changes to your work routine: Do you spend much time standing or sitting? Remember to take a break and include more movement into your regimen. Taking a few minutes to take a break from your regular position will help reduce the pain.
5) Get high-quality diabetic socks: Diabetic socks are great for many reasons. Besides being infused with high-quality materials such as bamboo and charcoal, which keep your feet free of excessive moisture and prevent infections, diabetic socks from Viasox also have extra padding. It'll relieve the weight on your feet, reducing heel pain.
6) Consider different treatment options: If you are interested in treatments, consider:
- Medication
- Steroid injections
- Physical therapy
- Shock wave therapy
- Surgery
Before starting any medication, consult your doctor first. According to Mayoclinic, ibuprofen naproxen sodium can help with pain and reduce inflammation. If your pain is severe, a steroid injection is an option to alleviate the pain immediately. Physical therapy is a great way to learn how to stretch to improve your leg muscles. Shock wave therapy will stimulate your heel to start healing. This is done by using low-frequency sound waves to stimulate the targeted area. If all the other methods fail, surgery is necessary. The procedure involves detaching the plantar fascia from the heel bone to relieve tension.
7) Stretch often: Besides actively working out, stretching is another way to strengthen your leg muscles and ligaments. Take a few minutes to do it; it will help reduce your heel pain.
Try out the Viasox product range
Please have a look at our broad collection of diabetic socks to see your options. You can see our customer reviews here. Many have shared how our fancy diabetic socks have helped alleviate pain in their legs and feet.
Feel free to contact us to learn more about our diabetic socks.





















